What if, instead of a daily balancing act of glucose monitoring, diet management, and insulin injections, a person with type 1 diabetes could just pop a pill for a short time and be done with insulin shots and finger pricks forever? Researchers at Novartis have taken the first step toward making this a reality with research focused on regenerating beta cells lost to the disease.
Recently they identified several compounds that cause human beta cells to replicate in the lab, a feat others had dismissed as impossible. The discovery, published online in Nature Communications on Oct. 26, suggests that it might be feasible to treat diabetes at its source.
“Most patients lose a lot of beta cells before they are diagnosed,” says Bryan Laffitte, last author on the paper and Director of Discovery Pharmacology at the Genomics Institute of the Novartis Research Foundation in California. “We took a chance that we would find something that would work to restore them in humans, and we’ve identified some promising compounds.”
Type 1 diabetes occurs when the immune system mistakenly destroys pancreatic beta cells, which secrete insulin to help the body absorb sugar from the blood and convert it to energy. Without these cells, patients must rely on injected insulin to survive. While people are surviving for much longer with modern medical tools, like continuous glucose monitors and insulin pumps, day-to-day management is still fraught with error even for the most vigilant of patients.
What these patients really need is a way to replenish their stockpile of pancreatic beta cells, which has usually dropped to 25% of the original level by the time of diagnosis. But human beta cells don’t regenerate easily. They stop replicating after infancy, and, based on the long track record of failed efforts to get human beta cells to proliferate, they are extremely resistant to it.
Laffitte and his team, however, were undeterred. They screened two million compounds, looking for agents that cause beta cells to replicate in a dish. After narrowing down the list of promising candidates, they gave two of the compounds to mice that closely mimic human diabetes. These animals with pancreatic damage have insufficient numbers of beta cells to manage their own blood sugar. Within two weeks, the mice were able to produce enough insulin to effectively control their blood glucose. The team later showed that the agents had actually doubled beta cell mass in these mice. In separate experiments, the researchers coaxed human beta cells transplanted into mice to proliferate.
“It was a really big deal for us to see the compounds work in models of human disease,” says Laffitte.
“These are the first screened compounds that have been demonstrated to stimulate proliferation of human beta cells,” says Richard Insel, Chief Scientific Officer of JDRF (formally known as Juvenile Diabetes Research Foundation).
Before jumping ahead to produce a drug, Laffitte and his team wanted to understand exactly what these compounds were doing inside the beta cells to make them replicate. Initial testing indicated that the most promising compounds hit and block the action of Dyrk1a, a protein kinase that’s involved in a molecular signaling pathway. Dyrk1a controls the location of another protein, a transcription factor called NFATc1, which activates many genes when in the nucleus of the cell. The compounds under investigation increased beta cell mass by coaxing NFATc1 into the nucleus.
It’s possible that the compounds identified by Laffitte and his colleagues could be tweaked to produce an experimental therapy, and the team is exploring this option. Dyrk1a, however, is active in more than just beta cells, so there are risks associated with moving forward. Another option is to find a target downstream of Dyrk1a in the molecular signaling pathway that is very specific to beta cells.
“We’re aiming for controlled cell proliferation, not proliferation all over the place,” says Laffitte. “We need to get the right cells to divide, replenish their mass and then stop without causing cancer.”
This work is part of a dual-pronged Novartis strategy to improve type 1 diabetes care that is also supported by JDRF. Alongside Laffitte’s efforts to restore beta cell mass so that patients can manage their own blood glucose levels, other Novartis teams are also looking for ways to protect beta cells from attack by the immune system.
“Ideally, we’re focused on intervening in multiple ways to really provide robust curative therapeutic solutions,” says Insel.
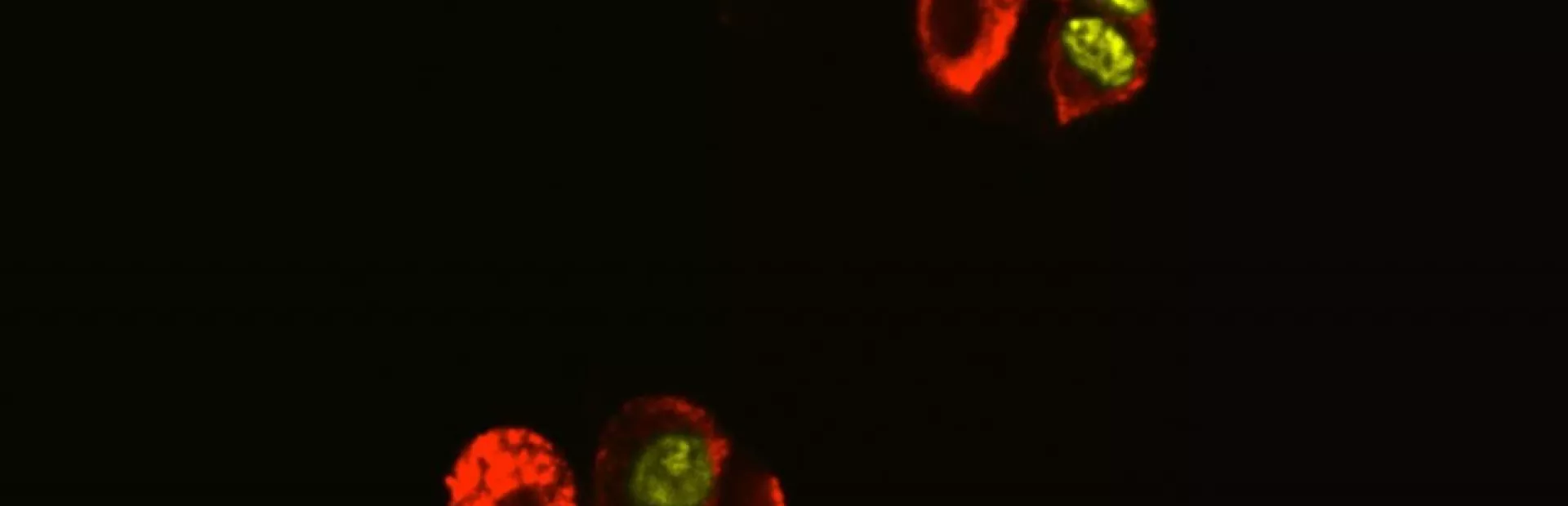
Researchers at the Genomics Institute of the Novartis Research Foundation coax beta cells to divide. Credit: Bryan Laffitte/Novartis
Discovery points toward regenerative medicine for type 1 diabetes.